Support the development of the TCCC project in Ukraine
Module 22: Cardiopulmonary Resuscitation in TFC
This module discusses cardiopulmonary resuscitation (CPR) considerations during the Tactical Field Care (TFC) phase.
Cardiopulmonary Resuscitation in Tactical Field Care

This module discusses cardiopulmonary resuscitation (CPR) during the Tactical Field Care (TFC) phase.
All Service Member and Combat Lifesaver training does not address the role of CPR. The Combat Medic/Corpsman will need to address any concerns about CPR in Tactical Field Care and apply the TCCC Guidelines.

There is one cognitive and one performance enabling learning objective for this module.
The cognitive objective addresses identification of the conditions of and considerations for cardiopulmonary resuscitation in Tactical Field Care.
The performance objective involves demonstrating bilateral needle decompression.
CPR was initially developed to try to maintain perfusion and oxygenation in a casualty with normal blood volume who was in cardiac arrest until defibrillation and advanced cardiac life support measures could be instituted. It was never envisioned as a viable treatment for cardiac arrest due to traumatic hypovolemia.
In fact, in civilian prehospital settings, even when a casualty is close to a trauma center, studies have repeatedly emphasized the futility of CPR. Most Emergency Medical Systems and professional societies recommended that CPR not be attempted for casualties who suffer a prehospital traumatic cardiac arrest, citing the large economic costs and the uniformly unsuccessful results. Even in casualties who arrived quickly at a hospital emergency room with a trauma team and underwent a thoracostomy, the survival rate was less than 2%.
On the battlefield, the delay in getting the casualty to definitive care makes it even less likely that a favorable outcome could be achieved. Dedicating limited resources to resuscitation attempts, or exposing responders to hostile fire while performing CPR, also compounds the situation and risks adversely affecting the outcome of other casualties. This further supports the decision to withhold CPR for casualties on the battlefield.
TCCC Guidelines state: “Resuscitation on the battlefield for victims of blast or penetrating trauma who have no pulse, no ventilations, and no other signs of life will not be successful and should not be attempted.”
Tension pneumothorax has been identified as a potential cause of non-hypovolemic cardiac arrest in trauma casualties, both in civilian and military research studies and retrospective reviews.
The data highlighting the improved casualty outcomes with needle decompression of the chest (NDC) is largely centered on casualties who were not in cardiac arrest, but there is some retrospective information to support its utility in pulseless casualties, as well. For example, in one retrospective study of 20,330 advanced life support paramedic calls, 12 patients in cardiac arrest were treated with NDC, and three of them had a return of cardiac output.
And there are anecdotal examples of success, including a casualty injured during a mounted IED attack in 2011 where the casualty was unconscious from closed head trauma and lost their vital signs during the prehospital phase. When a bilateral needle decompression was done in the emergency room there was a rush of air from a left-sided tension pneumothorax and a subsequent return of vital signs.
The Armed Forces Medical Examiner’s office has also identified undiagnosed tension pneumothoraxes in autopsies of casualties from our recent conflicts.
Based on this information, several authors and subject matter experts recommend that for combat trauma casualties without a pulse, bilateral NDCs should be performed due to the potential benefit and clear absence of additional harm. As a result, the TCCC Guidelines now state: “… casualties with torso trauma or polytrauma who have no pulse or respirations during TFC should have bilateral needle decompression performed to ensure they do not have a tension pneumothorax prior to discontinuation of care.”
Not all casualties on the battlefield are victims of blast or penetrating trauma. Cardiac arrest in the absence of blast or penetrating trauma may warrant consideration for initiation of CPR.
For example, in severe cases of hypothermia, a casualty can lose vital signs but regain them once they have been actively warmed; and if CPR is initiated, their outcome may be improved. Similarly, near-drowning victims may experience cardiac arrest. Another situation you could encounter is electrocution, in which a return of normal cardiac activity may be delayed, but occur even in the absence of defibrillation. These, and other non-traumatic instances of cardiac arrest, may lead you to consider initiating CPR.
However, the same potential drawbacks previously mentioned apply in these cases, as well. If the situation is not safe, the responders may be at risk of becoming casualties while performing CPR. The resources that need to be dedicated to proper CPR are significant, to include multiple people to do compressions and provide respirations, perhaps over a significant amount of time, depending on the evacuation and transfer options. Mission success should not be compromised, and the Combat Medic/Corpsman will need to weigh all of these issues when making a determination about initiation and cessation of CPR attempts.
Not covered in this discussion, but important to understand, is that the Tactical Evacuation Phase TCCC Guidelines state: “CPR may be attempted during this phase of care if the casualty does not have obviously fatal wounds and will be arriving at a facility with a surgical capability within a short period of time. CPR should not be done at the expense of compromising the mission or denying lifesaving care to other casualties.”
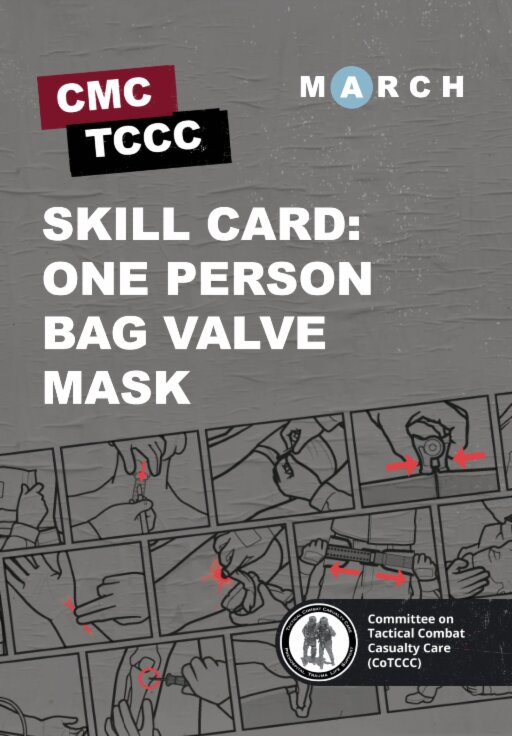
This is the same video that was shown in the Respiration module. Since it’s been a little while since we watched it, we’ll take some time to review the procedure prior to the skills station.
BILATERAL NEEDLE DECOMPRESSION OF THE CHEST (VIDEO)

PDF Bilateral Needle Decompression of the Chest Skills Card

During this module, we went over cardiopulmonary resuscitation in TFC.
We highlighted that CPR should not be initiated for a casualty who suffers blast or penetrating trauma with no pulse, respirations, or signs of life. But casualties with torso trauma or polytrauma who have no pulse or respirations should have bilateral needle decompression performed. And in some non-traumatic conditions, CPR should be considered.
The skill station reinforced the procedures for performing a bilateral needle decompression of the chest.
To close out this module, check your learning with the questions below (answers under the image).
Check on learning
Answers
Should you initiate CPR for a casualty with blast or penetrating trauma who has no pulse, respirations, or signs of life?
Resuscitation on the battlefield for victims of blast or penetrating trauma who have no pulse, no ventilations, and no other signs of life will not be successful and should not be attempted.
When should you perform a bilateral needle decompression of the chest?
Casualties with torso trauma or polytrauma who have no pulse or respirations during TFC should have bilateral needle decompression performed to ensure they do not have a tension pneumothorax.
In what circumstance might you consider CPR in the Tactical Field Care phase?
In severe cases of hypothermia, near-drowning victims, electrocution, or other non-traumatic instances of cardiac arrest.

You can discuss this material on the TCCC forum